Cranial nerve testing is BORING!
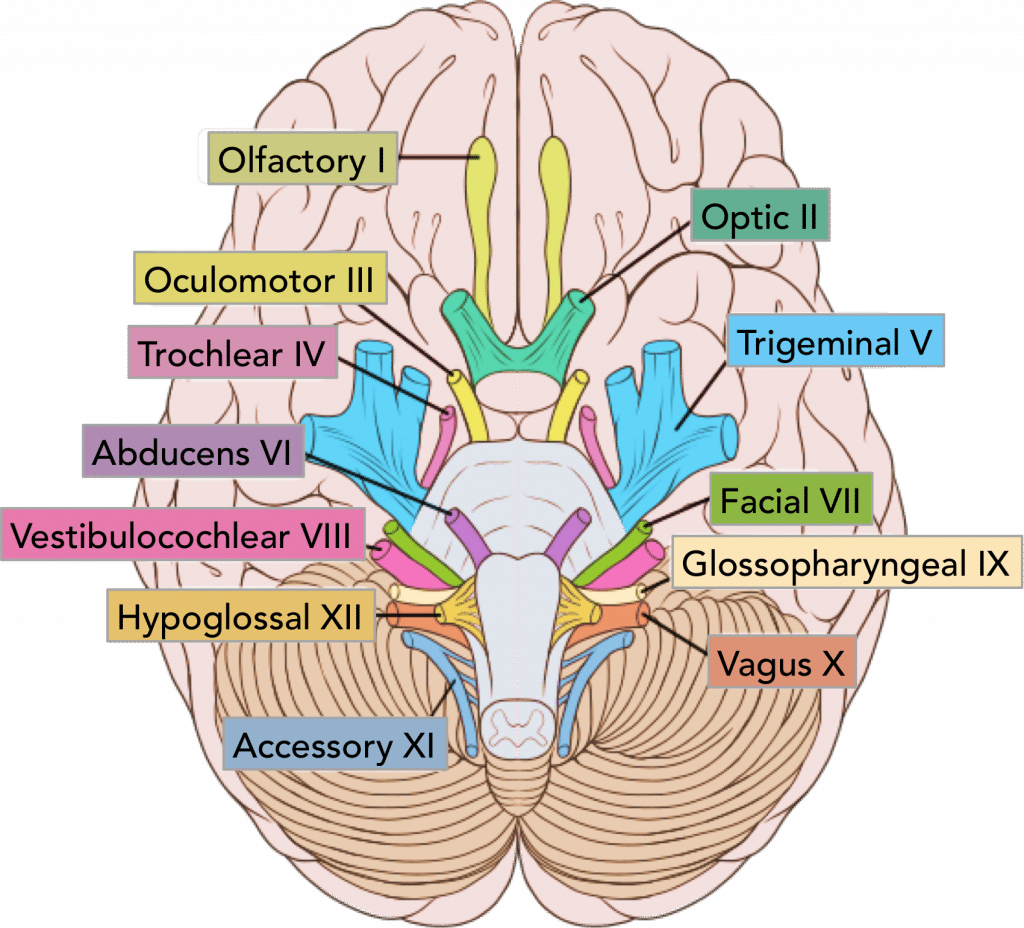
In entry-level physical therapy education, I remember learning (well, memorizing at the time) the cranial nerves. We did everything we could to remember it including the most entertaining mnemonics 
It never “stuck” with me to include this in daily clinical practice examination until I followed through with my Fellowship Program and specifically used it in a manner to rule-out conditions, specific conditions at that.
I enjoyed reading an article entitled, “Extracranial internal carotid artery aneurysm presenting as symptomatic hypoglossal and glossopharyngeal nerve paralysis” in The Journal of Laryngology & Otology in 2004. Even though “old” in today’s standards for evidence-based practice, I want to point out the concepts that arise from the clinical reasoning and its relationship to Cranial Nerves and the Internal Carotid Artery.
One concept I always push in our Cervicogenic Dizziness Course is that we need to be vigilant on the entire cervical vascular system and not just screening for Vertebrobasilar Insufficiency. This ultimately means we need to know about signs/symptoms and clinical characteristics of disorders to the Internal Carotid Artery. We can therefore, make sure we rule-out other sinister conditions to then aid in ruling-in Cervicogenic Dizziness as the diagnosis.

Just as described in our Optimal Sequence Algorithm, the first step prior to even assessing the vascular system, especially any mechanical disruption, is to go “back to basics”.
This involves initially examining the cranial nerves, especially the ones that may be affected first in a patient presenting with internal carotid artery dysfunction.
A negative finding on cranial nerve examination is one of the presenting clinical findings that led the team in this paper to perform an ultrasound on the neck and then refer for MR imaging.
You may ask what led to performing cranial nerve exam. Here you go:
Here are the paper highlights:
Subjective
- After a patient went to chiropractor for 3 visits 1 month prior, she self-admitted to ENT office for painful swelling in jaw .
- She had several bouts of dizziness associated with turning her head to her left.
- She had bouts of light-headiness.
- She also developed loss of hearing in her left ear.
Objective
- Odd sensation with swallowing
- Marked tongue deviation to the right side with tongue protrusion

So how does this relate to Cervicogenic Dizziness?
- The subjective findings above could mean mechanical or non-mechanical source of symptoms but objective findings indicate a cranial nerve palsy response to cranial nerve testing (specifically hypoglossal and glossopharyngeal).
- Patient could have self-admitted to a physical therapy office instead of ENT, so ultimately we need to be able to fully examine someone with initial thoughts of non-mechanical symptoms unless proven otherwise.
- Positional dizziness, such as turning head to the left, are typical symptoms associated with the diagnosis of Cervicogenic Dizziness.
- Lightheadiness is a typical symptom associated with the diagnosis of Cervicogenic Dizziness.
- She had a recent minor trauma, which in this case, was a trip to the chiropractor with assumption of a manipulation performed.
- Instead of seeing another clinician, she could have simply had a recent minor trauma from looking up, played golf, or even had a concussion or in a car accident.
Even though the authors suggest there was a correlation with chiropractic manipulation prior to patient seeing ENT, it cannot be proven that the procedure was the cause of her cranial nerve palsy. In fact, her attacks of lightheadiness and pain worsened after initial visit to the ENT, who prescribed anti-biotics! Another post on this coming in the future.
Nevertheless, we recommend clinicians screen appropriately with subjective and objective examination procedures, especially if someone is presenting with symptoms of lightheadiness, dizziness and/or vertigo.
You can learn more about the screening and treatment process of Cervicogenic Dizzinesss through Integrative Clinical Concepts, where the author and his wife, a Vestibular Specialist, teach a 2-day course. Pertinent to this blog post, the first day provides the most up-to-date evidence review from multiple disciplines to diagnose through the “Optimal Sequence Algorithm” to assist in ruling out disorders and ruling in cervical spine, including determining if single or double entity exists.
If you would like to host a course for your staff (either a vestibular, neuro, sports or ortho clinic), please do not hesitate to contact me at harrisonvaughanpt@gmail.com for prices and discounts.
Authors
Harrison N. Vaughan, PT, DPT, OCS, Dip. Osteopracic, FAAOMPT
Instructor: Cervicogenic Dizziness for Integrative Clinical Concepts
Danielle N. Vaughan, PT, DPT, Vestibular Specialist
Instructor: Cervicogenic Dizziness for Integrative Clinical Concepts
Keeping it Eclectic...

















Post a Comment
Post a Comment