My clinic serves a low socioeconomic city area. Now, I am sure that there are any number of stranger work conditions, treating in a gang-controlled area, for example, but the conditions and problems of low socioeconomic status (SES) are a niche unto themselves.
Almost everything "straight ortho PT" gets thrown out. Low SES throws a wrench in the gears.
From our clinic perspective, it means lots of un-managed chronic conditions, high cancellation rate and difficulty with adherence to HEPs. Transportation to the clinic is a large issue because it has a cost (either money or time) to the patient that is often a deterrent to coming to appointments. People prefer not to wait for the bus in the cold.
From a clinician perspective, it can mean treating back-to-back pain catastophizing patients, chronic/persistent pains and allodynia/hyperalgesia patients. High levels of fear avoidance behaviors and chronic pain habituation. It means a lot of assessing, maneuvering and adjusting to find ways in. It's a high mental load.
From the patient's perspective it means trouble getting to appointments, as mentioned, spending money you don't have (on transport or co-pays) and being in an environment that is new and non-typical. All uphill battles.
And #cashPT? If you mean literal cash (no bank accounts) and a budget of $500 month then yeah... sure, #cashPT. Most only come because it is paid for under their 3rd party payer (insurance, lawyer, etc).
Direct Access? Yes, they were Directly told to Access our clinic by their physician.
There is more to say here, but I must say that I am rarely treating an elbow or a knee. I am treating a person. And with low SES the complexities emerge. These are the people who need therapeutic neuroscience education. These people need behavioral intervention and patient education on lifestyle choices. But the problem emerges- A crushingly powerful statement by Mike Eisenhart says it all: "[We] are trying to help unhealthy people... with tactics that are meant for healthy people." I have well developed analogies and stories for pain, I have movements and exercises to improve tissue qualities... they don't relate... and I can't relate.
The process of communication presents many challenges. When I explain pain processes we get stuck early on. Words like "neuron" are not sticking. If there is some tool/device I would recommend I say, "you can pick one up on Amazon." "What's Amazon?" is the response. I offer to use their cellphone to video an HEP clip of themselves, most often, the patient pulls out a flip phone or no phone.
If trouble with essential patient education is a struggle then let's fully disregard the small chit-chat that occurs in many outpatient clinics about Thanksgiving or Black Friday deals... the chat about what you or they are doing this weekend. The conversations often lead no where and you end up alienating people if you treat this as a typical interaction. Your patient may not have family, Black Friday is a thing people in her community just don't do, and nothing is going on this weekend.
Patient education is one of our greatest tools. Teaching an individual that did not get an education, or did not learn how to learn well really throws a wrench into the system. If in 5th grade your patient got 'D's, indicating 60% of understanding, well that's about what you get with health information as well: a 'D' in health literacy. Education is an uphill battle.
These factors set the patient up to learn from us that they have "strange problems" with their body. It can turn into a "Game of Telephone" between two people. In addition to all the "bone-on-bone" and "you'll have back pain for ever" comments, let me share just a few things that I hear:
"I've got a nerve pressing on my lumbato bone"
*Patient rubbing his knee: "It hurts here, in my lymph noids"
"I've got the plantitis inflamination"
"They say my menicles is torn."
After you chuckle to yourself for a minute, the sad reality sinks in. This is the view of their body. A large gap in vocabulary, not well bridged by us in health care. Let alone the vocabulary, think of the self-image contained in their sensory homunculus based on what they think they know about themselves. Their body perception. Additionally, we know that 'menicles' means 'meniscus' and what a meniscus is... but let's not assume that vocabulary is the only thing not translated in the conversation with health providers. What do they think a menicles is?
Those that need it the most are the hardest to reach. I'm not pointing this out to say that "my patients are the hardest" or whatever. Because the same rehab principles apply across the board. It's just that it's much more "physical THERAPY" than "PHYSICAL therapy."
This is not to frame this population as not smart. Surely oppression drives the wise into madness - Ecclesiates 7.7 If the culture of your life was of an external locus of control, all wind and no sail, a wall in your path... then it is often the most bright that are disturbed the most. You see the frenzied search for solution in their eyes. But the behavioral and cultural coping strategies are not there... not there, to meet the complexities of the model social human. So behavioral boundaries can be seen as well.
While the environment may not encourage growth, we also see the individual who's choices have placed them in this environment. We must indeed not ignore both nature and nurture. Un-managed or un-addressed mental health concerns, across the spectrum, end up in this SES genre.
The persistence of conditions and low understanding of self-management is often clear. They enter the system late, or they enter the system at wrong entry points (ER visits for diabetic ketoacidosis instead of a PCP for consistent A1C testing). Some say that these problems stem because there is not money in helping those in the low SES category. Perhaps, based on payer types, but a typical shoulder or knee may improve in 4-10 visits, while those with multiple co-morbidities, slow healing processes and long standing pains will easily be double that to see progress, if they progress at all. More visits for the "same" (not really) shoulder pain. An ER charge of $2000 or an MD/DO visit for $150. Perhaps there is more money to be made off this population... in a way... so I don't know if it's all that clear.
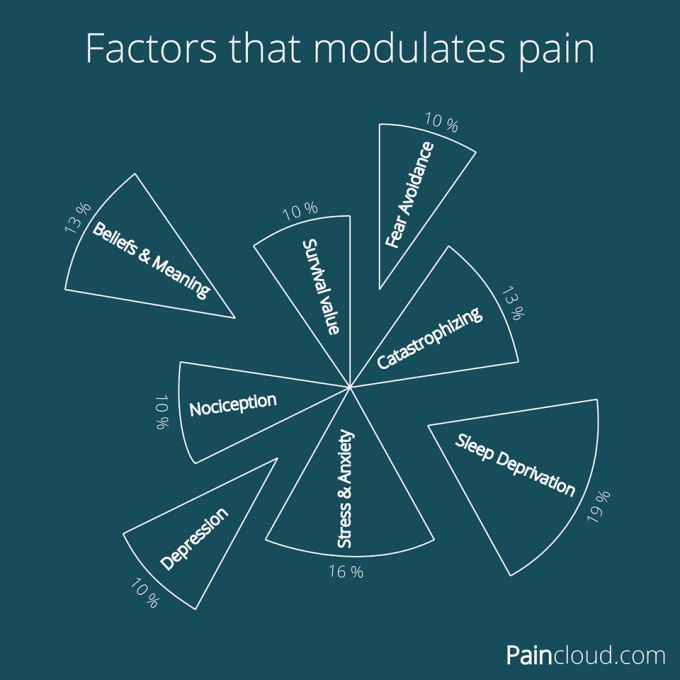
So, those traditional tissue treatments, the knee mobs etc, are starting from behind and have to play catch-up to make a difference in this person's life. If improved feeling and mood is influenced by many biopsychosocial factors (as seen above in PainCloud's photo) then 10 minutes of manual and 20 minutes of repeated motion and mobility drills will only dent the surface. Yes it helps, but not in the way you were told in school or in that course.
Another wrench in the management of this population is adding Value to their experience and customer satisfaction type concerns.It is hard to gauge what is to be valued by this patient, because it may not be what we value. We may value a quick 6 visits and return to function. They may be expecting medicine... or a shot... or one visit of magical hotpack/estim to cure their pain. They may value interaction with another person and someone to listen for many many visits.
Value is perception (not tied to any objective shared reality). Additionally, at a co-pay of $5/visit, no amount of attention, education and movement therapy may be worth it. As H.D. Thoreau says: The price of anything is the amount of life you exchange for it. If there are no goals imaginable to the patient that they are willing to work towards, that they are willing to struggle through the therapeutic process for... well, then "scheduled PT visits" are an amount of life they they do not wish to exchange for some future promise of relief.
By this point, many of these people (not isolated to low SES here) are skeptical of the Health Care System, they have been passed around from specialist to specialist, not really understanding what each one does, what the specialist did to them or what was wrong and now what was "fixed." The interaction often starts out on the defensive. The "I don't know why I'm here" and the "It hurts, what can you do about that?" I've been taking morphine for 6 years, they help "a little," what are you going to do to help me? It's a mix of "all they did was give me meds" verses "I need my meds, that's the only thing that helps." It's an uphill battle against the preconceived expectation of frustration.
In the end, the population needs much more than we can give. We are but a brush stroke on the canvas of their life. It is difficult to make change in even an hour interaction, let alone 30 minutes. (Sorry to the PTs and patients who must conduct this process in 15 minute blocks).
A healthcare team approach is good, a community approach is better. I certainly don't have answers, but knowing questions and problems is valuable as well. Enter all the analogies about how it's easier to keep something running clean with small efforts VS having to do a big overhaul on an un-maintained machine. It's exhausting to fight fires compared to checking the fire extinguisher.
Yes a future answer is early access, community engagement and changing societal behavior towards healthy choices. I worry though... are "[We] trying to help unhealthy people... with tactics that are meant for healthy people." Will we relate?
-Matt Dancigers, DPT
Image Credit
Interested in live cases where I apply this approach and integrate it with pain science, manual therapy, repeated motions, IASTM, with emphasis on patient education? Check out Modern Manual Therapy!
Keeping it Eclectic...













Post a Comment
Post a Comment